Cardiology – General Cardiology Fellowship
Overview
The Brown Fellowship in Cardiovascular Disease is a clinically and academically rigorous program that prepares fellows to function as experts in the field of general clinical cardiology, as well as providing a solid foundation for subspecialty training and careers in cardiovascular research. Brown’s dedicated faculty are committed to fostering an atmosphere of collegiality. Essential tenets to Brown’s teaching philosophy include the availability of faculty, the creation of a positive and supportive learning environment, a team approach to patient care and research, and the ability to individualize curriculum to support each fellow’s career goals.
 Katharine A. French, MD, MPH
Katharine A. French, MD, MPH
Director, General Cardiology Fellowship Program
Director, Women’s Cardiac Center
Current Fellows
Click here to view our 2024 – 2025 Fellows Photoboard.
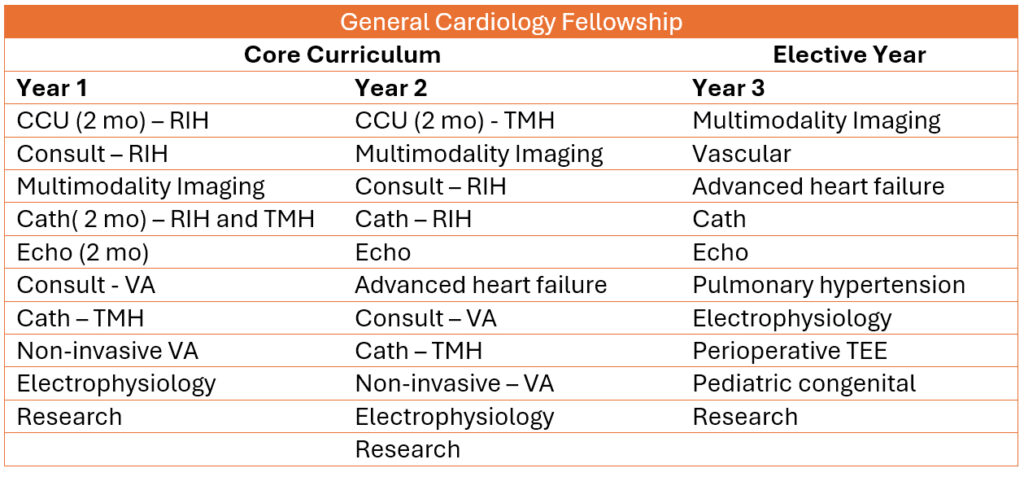
Curriculum: The 2+1 Model
Brown University’s educational philosophy emphasizes the importance of an “open curriculum” to support the individual needs and interests of its learners. The Brown General Cardiology Fellowship embraces this philosophy in it’s 2+1 curriculum model. The 3-year fellowship is broken down into two years of core clinical curriculum followed by one year of elective time. In the third year, the fellow may select to focus on advanced training in a number of areas including noninvasive imaging, invasive cardiology, electrophysiology and/or cardiovascular research.
Core Rotation Descriptions
CCU – RIH and TMH
During the CCU month, under the supervision and guidance of the attending cardiologist, the fellow leads a team of residents and medical students whose primary objective is to care for patients with acute cardiovascular illnesses. The CCU month is an immersion into cardiac critical care where fellows are involved in all aspects of care including management of acute coronary syndromes, decompensated heart failure, severe valvular disease and unstable arrhythmias. Fellows are responsible for evaluation and triage of acute unstable cardiac conditions in the emergency room as well as the bedside procedural needs of CCU patients (placement of transvenous pacemakers, PA catheters and management of hemodynamic support devices including intra-aortic balloon pumps and Impellas).
Multimodality Imaging
Fellows spend at least 3 months over the course of their fellowship rotating through our non-invasive imaging labs. Imaging modalities include nuclear cardiology, cardiac MRI and cardiac CT. Fellows receive training in SPECT and PET camera design and operation, radiation safety, pharmacologic stress agents, and metabolic and amyloid imaging. Within the realm of cardiac CT and MRI, fellows work with cardiac and radiology faculty as well as technicians to gain exposure and competency in imaging protocols and study interpretation with a focus on integrating multimodality imaging results with clinical data to guide clinical decision making.
Consult – RIH, TMH and VA
During the cardiology consultative months, the fellow leads a team of residents and medical students, under the supervision of the attending cardiologist, to provide cardiac consultations on inpatients admitted to general medical, surgical and subspecialty services. Fellows are exposed and gain experience managing a diverse range of cardiac conditions. Fellows are also responsible for cardiac consultative services at neighboring Women and Infants’ Hospital, providing exposure to the field of cardio-obstetrics.
Cath – RIH and TMH
The cardiac catheterization labs at both RIH and TMH see high volumes of cases, providing general fellows with ample opportunities to gain experience in all aspects of interventional cardiology. General fellows participate in acquiring, interpreting and reporting results from invasive hemodynamic and angiographic assessments, as well as therapeutic interventions. Fellows play a key role in the care of cardiac patients before, during and after procedures as dictated by their level of experience, including case selection and procedural planning.
Echo
The echo rotation is a lab-based rotation that involves all aspects of acquiring and interpreting echocardiographic studies. First year fellows begin with gaining hands-on experience, learning to perform complete transthoracic studies under the guidance of our experienced technicians. Subsequent rotations focus on interpretation of transthoracic studies followed by triage, performance and interpretation of transesophageal studies. Fellows may apply for advanced training in echocardiography during their third year of fellowship (achieving COCATS level 3). Fellows selected for this pathway participate as members of our structural heart team, gaining the interventional echocardiographic skills necessary to guide an array of catheter-based structural heart procedures.
Non-Invasive VA
The non-invasive month at the VA provides fellows the opportunity to perform and interpret a wide range of cardiac testing and procedures. Fellows responsibilities include weekly supervision of treadmill stress testing, EKG and Holter monitor interpretation, and interpretation of nuclear stress tests and echocardiograms. They perform transesophageal echocardiograms, cardioversions and outpatient right heart catheterizations.
Electrophysiology
Under the supervision of the attending electrophysiologist, the general fellow runs the EP inpatient consultative service, providing consults for patients on the cardiology services as well as non-cardiac inpatient services. Fellows are trained in pacemaker and ICD indications and interrogation, complex arrhythmia assessment and management ,and placement of temporary transvenous pacemakers. They have the opportunity to spend time in the EP lab gaining exposure to device placement and ablation procedures.
Advanced Heart Failure
During the heart failure month, fellows gain experience in inpatient consultative management of patients with advanced heart failure. Patients seen by this service include acutely ill patients in the intensive care units on inotropic and mechanical support, all patients with LVADs or prior heart transplants, new heart failure with severely reduced systolic function and patients with frequent readmissions for heart failure. Fellows also attend weekly clinic sessions in our advanced heart failure center.
Research
Whether a fellow chooses to pursue a career in academic or clinical medicine, familiarity and experience with research methods and analysis is essential for fostering intellectual inquisitiveness and critical thinking – both of which are essential characteristics of master clinicians. For this reason, fellows in the general cardiology fellowship program are expected to participate in cardiovascular research during their 3-year program. One month during the first and second years of training provides dedicated research time. Fellows can elect to dedicate additional time to research activities during their 3rd year.
Continuity Clinic
Fellows attend a general cardiology continuity clinic, under the supervision of our faculty, averaging one half-day per week over the course of their 3-years. Continuity clinics are located at one of Brown University Health offices in East Providence and at the Providence VA Medical Center. During the third year, fellows have the option of expanding their outpatient cardiology experience to include time rotating through our subspecialty cardiac clinics such as advanced heart failure, structural heart, interventional cardiology, women’s cardiology, congenital heart disease, electrophysiology, lipids, and cardio-genetics.
Lecture Series and Conferences
Conferences and lectures are an integral part of the cariology fellowship and are attended by fellows and faculty. Our faculty provides a core didactic lecture series which spans the academic year. Cardiology Grand Rounds take place on a weekly basis and are comprised of nationally-recognized invited speakers, M&M cases, and senior fellow presentations. Technical conferences for ECG interpretation, echocardiography, and catheterization, in addition to journal club and subspecialty conferences complement the core curriculum throughout year.
Training Sites
Rhode Island Hospital is a not-for-profit, 719-bed, acute care hospital. It is the largest hospital and the only Level I Trauma Center in Rhode Island. It is also the principal teaching hospital for the Alpert Medical School of Brown University.

The Miriam Hospital is an outstanding 247-bed academic community hospital located on Providence’s East Side. The Miriam Hospital has been ranked the best hospital in Rhode Island and southeastern Massachusetts by US News and World Reports and has received the Magnet Award for Excellence in Nursing Services five times in recognition of its outstanding nursing culture. The hospital is known for its cardiac care at the Cardiovascular Institute, as an award-winning Stroke Center, as a regional orthopedic referral center with the Total Joint Center, as well as for programs in bariatrics, urology, and many other services.

The Providence VA Medical Center is a 73-bed facility that delivers a broad range of services in medicine, surgery, and behavioral sciences. Cardiac services include a full range of non-invasive imaging modalities including echo, nuclear and MRI in addition to a stress lab and invasive vascular lab.

Application Information
We participate in the ERAS application process. For information on application timeline, please go to: https://students-residents.aamc.org/training-residency-fellowship/article/eras-fellowship-timeline/
Note: All first-year Cardiology Fellows will start at the PGY4 level regardless of prior training.
If you have any questions, please contact:
-
Jane Freer
Cardiology Program Coordinator
Rhode Island Hospital/Brown University Health
593 Eddy Street Providence, RI 02903
Email: JFreer@BrownHealth.org
Tel: 401-444-8689
Fax: 401-444-4652
About Us
The Department of Medicine at Alpert Medical School is comprised of eleven distinct Divisions. These Divisions, working in conjunction with the community doctors who comprise our Primary Care offerings, provide patients with an outstanding level of care both within the Brown affiliated hospitals and throughout several community-based clinical locations. In addition to patient services, several of our Divisions offer exceptional programs for Residents and Fellows within their designated areas of expertise.
How To Reach Us
Office of the Physician-in-Chief
Louis B. Rice, MD
593 Eddy Street
Providence, RI 02903
Louis B. Rice, MD
593 Eddy Street
Providence, RI 02903